
These patients had been admitted to the Department of Poisoning and Occupational Diseases, QILU Hospital of Shandong University (Jinan City, China) between Januand December 31, 2021. Six patients with AOPP who suffered a cardiac and/or respiratory arrest and were successfully resuscitated on-site were selected as research participants. In this study, we analyzed the clinical data of patients with AOPP who experienced cardiopulmonary arrest and successful cardiopulmonary resuscitation (CPR) on-site and summarized the clinical characteristics and prognostic factors of the aforementioned disease.

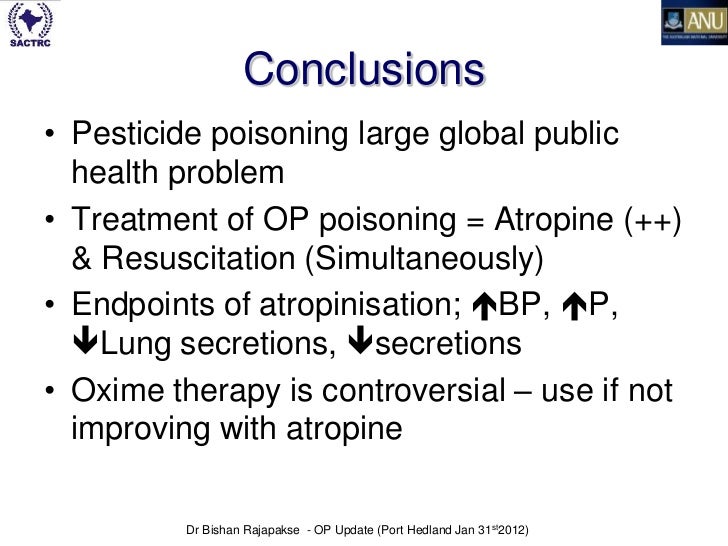
However, AOPP-related cardiac arrest is rarely reported. Common symptoms of AOPP include central nervous system and neuromuscular complications, with cardiopulmonary arrest being the most serious complication and often having a very poor prognosis ( 6, 7). OPs cause damage to multiple organs through cholinergic and non-cholinergic effects ( 5). In China, AOPP cases comprise nearly 50% of all poisoning cases, with case fatality rates of 3–40%, comprising over 80% of all poisoning deaths ( 3, 4). Acute organophosphorus pesticide poisoning (AOPP) is a major life-threatening toxic disease in the rural areas of developing countries ( 1, 2). Some organophosphorus pesticides (OPs) are extremely poisonous and cause rapid intoxication-induced death with minimal ingestion or exposure. This study provides useful guidelines for the treatment of similar cases in the future. Application of atropine and pralidoxine in a timely manner after cardiac arrest following AOPP is the key to successful treatment.

Cardiac arrest can occur in patients with severe AOPP for whom antidote administration was insufficient or not timely. This, along with their death, might have been related to their prognosis. The last two patients had severe pancreatic injuries and disseminated intravascular coagulation. Four patients recovered and were discharged from the hospital, one died in our department, and one was transferred to a local hospital and died there 2 h later. Five patients had not undergone hemoperfusion therapy before cardiac arrest, and all six were treated with atropine during cardiopulmonary resuscitation and subsequent pralidoxine. This study included six cases of patients with AOPP in addition to cardiac arrest in four cases, cardiac arrest occurred <12 h after ingestion, and in two, cardiac arrest occurred more than 48 h after ingestion. We conducted a descriptive analysis of the clinical manifestations, rescue strategies, and prognosis of patients with AOPP who had experienced cardiac arrest and successful cardiopulmonary resuscitation. This retrospective study was conducted in our department in the years 2018–2021. Therefore, this study aimed to explore the prognostic factors and effective treatments of AOPP-related cardiac arrest.


 0 kommentar(er)
0 kommentar(er)
